At KHOOR, we’re tackling a critical health issue: smoking during pregnancy. Financial incentives for smoking cessation in pregnancy have emerged as a promising strategy to address this problem.
We’ll explore the effectiveness of these programs and their potential to improve maternal and infant health outcomes. Our analysis covers current initiatives, research findings, and implementation considerations for policymakers and healthcare providers.
What Are Financial Incentives for Quitting Smoking During Pregnancy?
Financial incentives for quitting smoking during pregnancy are monetary or material rewards given to expectant mothers who stop smoking successfully. These programs motivate pregnant women to quit by offering tangible benefits for their efforts.
Types of Incentives
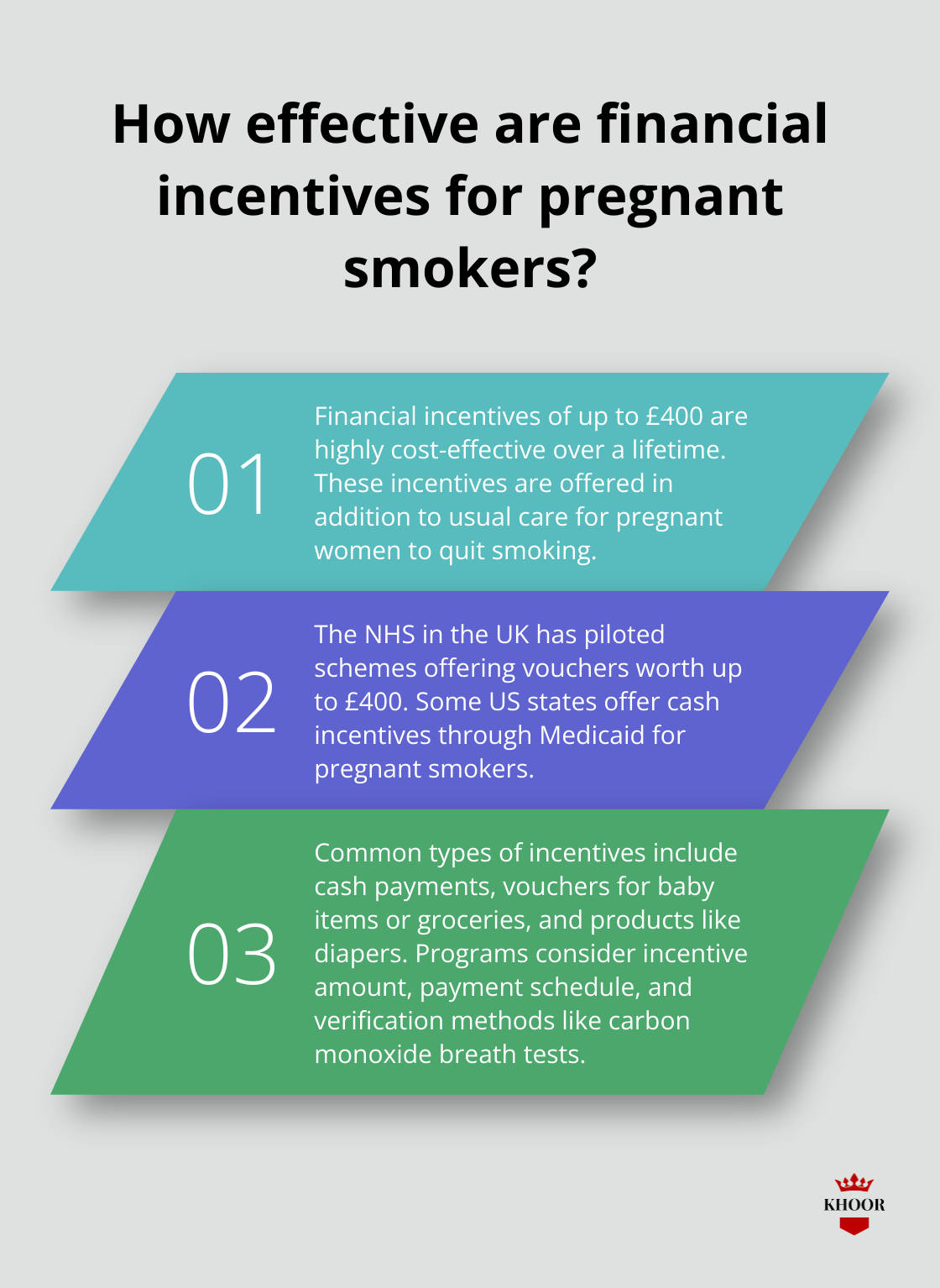
The most common types of incentives include:
- Cash payments: These are straightforward and allow recipients to use the money as they see fit.
- Vouchers: Often for baby-related items or groceries, directly benefiting the mother and child.
- Products: These might include items like diapers or baby clothes.
Effectiveness of Incentive Programs
Research shows these incentives can be highly effective.
A study found that offering up to £400 financial incentives, in addition to usual care, to support pregnant women to stop smoking appears to be highly cost-effective over a lifetime.
Global Initiatives
Several countries have implemented financial incentive programs:
- UK: The NHS has piloted schemes offering vouchers worth up to £400.
- US: Some states offer cash incentives through Medicaid.
- France: A study involving pregnant smokers across maternity wards tested the effectiveness of vouchers for maintaining abstinence.
Program Design Considerations
When designing these programs, it’s important to consider:
- Incentive amount
- Payment schedule
- Verification methods (e.g., carbon monoxide breath test)
Programs should also address potential ethical concerns, such as fairness to non-smokers and the risk of incentivizing unhealthy behaviors.
Cost-Effectiveness Analysis
While the upfront costs of these programs can be substantial, they often prove cost-effective in the long run.
The Smoking Cessation in Pregnancy Incentives Trial (CPIT III) highlighted the lack of evidence for effectiveness of financial incentives to help pregnant smokers quit, as noted in UK national guidelines. This includes a research recommendation for further trials.
As we explore the effectiveness of financial incentive programs, it’s important to understand how they compare to other smoking cessation methods and their long-term outcomes for mothers and babies.
Do Financial Incentives Work for Pregnant Smokers?
Remarkable Success Rates
Financial incentives appear to be effective in promoting smoking cessation in pregnancy. A study in the journal Addiction revealed that offering up to £400 in vouchers significantly increased quit rates among expectant mothers. The Smoking Cessation in Pregnancy Incentives Trial (CPIT III) showed that women who received financial incentives were more than twice as likely to quit smoking compared to those who received standard care alone.
Impressive Statistics
The effectiveness of financial incentives becomes clear when examining the data. In the CPIT III trial, 26.8% of pregnant women who received vouchers quit smoking, compared to just 12.3% in the control group. This translates to an odds ratio of 2.63, indicating that financial incentives more than doubled the chances of successful smoking cessation.
A review analyzing multiple studies found that incentives increased smoking abstinence rates by 2.38 times at up to 24 weeks postpartum. This suggests that the benefits of financial incentives extend beyond pregnancy, potentially leading to long-term smoking cessation.
Outperforming Traditional Methods
Financial incentives have shown superior results when compared to other smoking cessation methods. Traditional approaches such as nicotine replacement therapy and counseling typically help 5-15% of pregnant smokers quit. In contrast, financial incentive programs have consistently demonstrated quit rates of 20-30% or higher.
A study in France (involving 460 pregnant smokers across 18 maternity wards) found that those offered vouchers for abstinence smoked 163 fewer cigarettes on average compared to the control group. This significant reduction in cigarette consumption highlights the potential of financial incentives to drive meaningful behavior change.
Long-Term Health Benefits
The impact of financial incentives extends far beyond immediate smoking cessation.
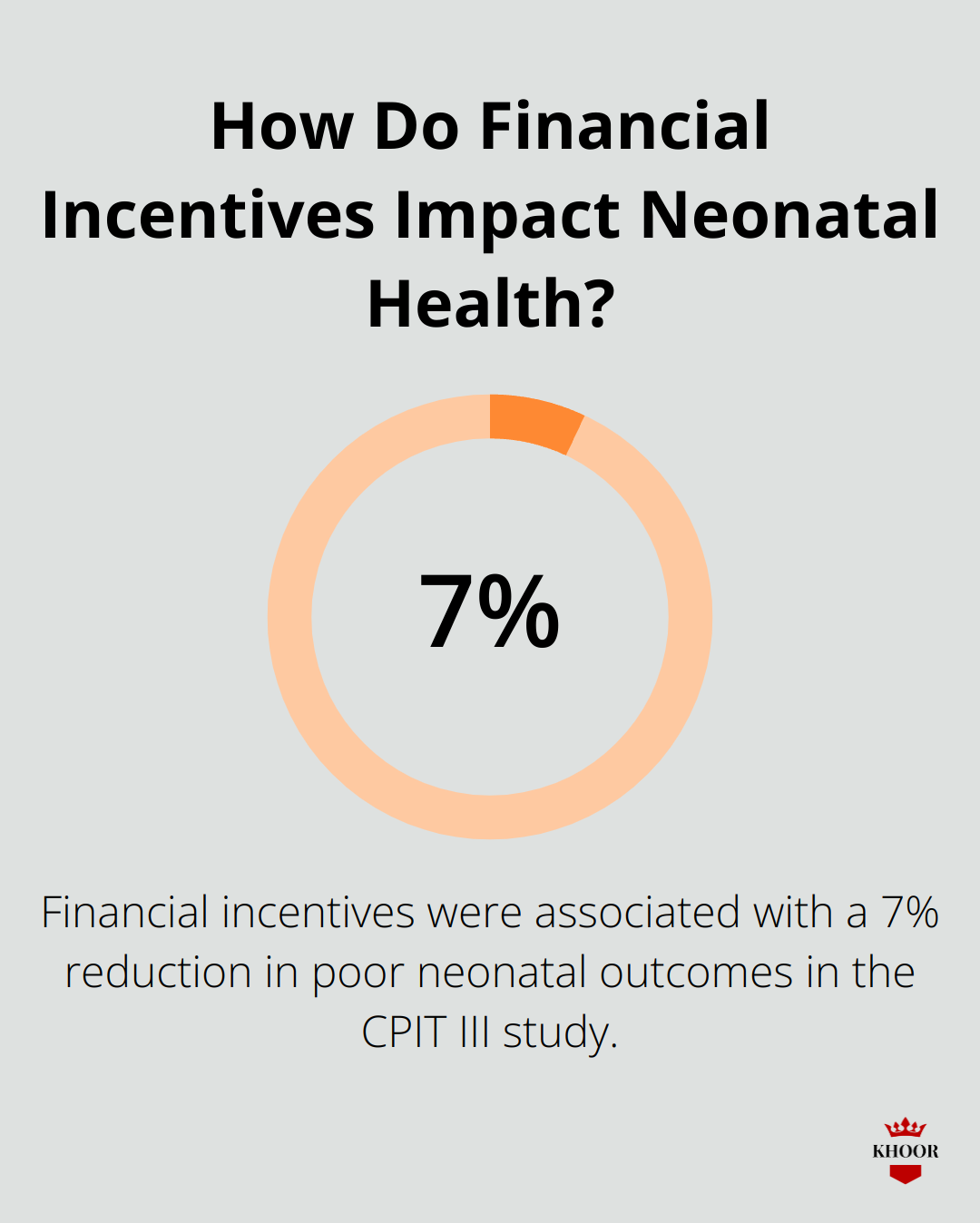
Smoking during pregnancy is related to complications and poor birth outcomes, including miscarriage, low birth weight, preterm birth, and stillbirth. The CPIT III study found that financial incentives were associated with a 7% reduction in poor neonatal outcomes (including transfer to neonatal units, congenital malformations, and perinatal death).
The long-term analysis of the CPIT III trial revealed that financial incentive programs are not only effective but also cost-saving. Over a lifetime, these programs resulted in an average cost saving of £37 and an increase in quality-adjusted life years (QALYs) by 0.171 for both mothers and infants combined. This demonstrates the substantial health and economic benefits of investing in smoking cessation incentives for pregnant women.
As we consider the effectiveness of financial incentives, it’s clear that they offer a powerful tool in the fight against smoking during pregnancy. The next step involves exploring how these programs can be implemented effectively and ethically to maximize their impact on maternal and infant health.
How to Design and Fund Effective Incentive Programs
Program Design Elements
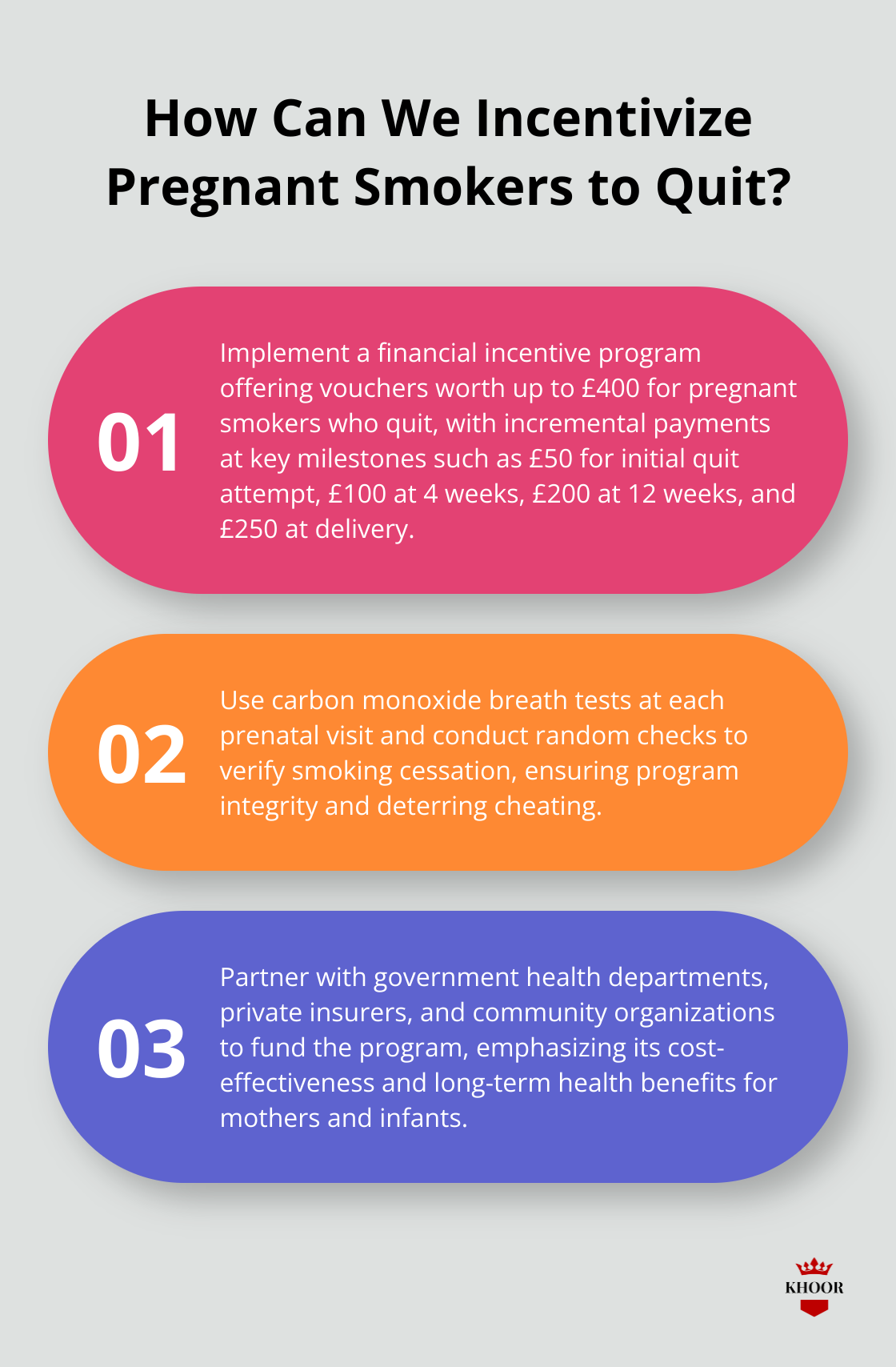
Successful incentive programs for pregnant smokers offer rewards between £400 to £600 throughout pregnancy. The
CPIT III trial, which showed significant success, provided vouchers worth up to £400. Programs should structure payments incrementally, with larger amounts for sustained abstinence. For instance, a program might offer £50 for the initial quit attempt, £100 at the 4-week mark, £200 at 12 weeks, and a final £250 for remaining smoke-free until delivery.
Verification plays a key role in program success.
Carbon monoxide breath tests (with a sensitivity of 33%) offer immediate results and deter cheating. Programs should conduct these tests at each prenatal visit, with additional random checks to ensure compliance.
Funding Sources and Cost-Effectiveness
The upfront costs of incentive programs may appear high, but they often prove cost-effective in the long run. The
CPIT III trial found that introducing financial incentives to usual care is a dominant strategy (cost-saving and QALY-gaining) using a life-time horizon.
Funding can come from various sources:
- Government health departments (primary contributors)
- Private insurers (understanding that preventing smoking-related complications reduces their payouts)
- Community organizations and charities focused on maternal and child health
Addressing Ethical Concerns
Critics often raise concerns about the fairness of rewarding people for quitting an unhealthy habit. However, the societal benefits of reducing smoking during pregnancy outweigh these concerns. To address fairness issues, some programs offer small rewards to non-smoking pregnant women for participating in health education sessions.
Another common criticism involves the potential for fraud. Robust verification methods (like the carbon monoxide tests mentioned earlier) are essential to maintain program integrity and public trust.
Programs must also ensure that incentives don’t inadvertently encourage women to continue smoking until pregnancy to qualify for rewards. Clear eligibility criteria (such as requiring participants to be smokers at their first prenatal visit) can mitigate this risk.
Implementation Strategies
To implement effective financial incentive programs, consider these strategies:
- Partner with healthcare providers to integrate the program into existing prenatal care
- Develop clear communication materials to explain the program to participants
- Train staff on program procedures and ethical considerations
- Establish a system for tracking participant progress and distributing rewards
- Regularly evaluate program effectiveness and make adjustments as needed
Implementing financial incentive programs for pregnant smokers requires careful planning and consideration. These programs (when designed thoughtfully and implemented effectively) can significantly improve maternal and infant health outcomes.
Final Thoughts
Financial incentives for smoking cessation in pregnancy have proven highly effective in improving maternal and infant health outcomes. Studies show significantly higher quit rates among pregnant women who receive monetary rewards, leading to long-term health benefits and cost savings for healthcare systems. The success of these programs depends on thoughtful design and implementation, with substantial rewards offered incrementally throughout pregnancy and rigorous verification methods to maintain integrity.
The long-term benefits of financial incentive programs outweigh the initial investment. Reduced smoking rates during pregnancy result in fewer complications, healthier babies, and decreased healthcare expenditures. Policymakers should consider integrating these programs into standard prenatal care to revolutionize smoking cessation efforts for pregnant women.
For those seeking a tobacco-free alternative,
KHOOR offers premium herbal cigarettes that provide a satisfying smoking experience without nicotine or tobacco. This option can help individuals looking to quit smoking or reduce their tobacco consumption. Financial incentives for smoking cessation in pregnancy represent a powerful tool in public health, investing in the health of future generations.